Tel: +86-19906868508
E-mail: info@sihanmed.com
Tel: +86-19906868508
E-mail: info@sihanmed.com
In modern minimally invasive medicine, a flexible endoscope is a sophisticated medical asset designed to navigate complex anatomical pathways without compromising structural integrity. Unlike traditional imaging modalities such as X-rays or MRIs, flexible endoscopy provides real-time, high-definition visualization of mucosal surfaces, enabling clinicians to detect early-stage pathologies that sub-surface imaging might overlook. However, the intricate mechanical design of these devices—consisting of thousands of micro-components—makes them highly susceptible to wear and tear. Understanding their core mechanics is the first step toward preventing costly downtime and ensuring patient safety.
A flexible endoscope is a medical device with a bendable tube and a camera, used to examine hollow organs like the stomach or lungs. Unlike a rigid endoscope, it navigates the body’s natural anatomical curves without discomfort—making it the gold-standard tool for both advanced diagnostics and interventional procedures. Yet, the constant mechanical stress of angulation and repeated exposure to harsh chemical disinfectants take a significant toll, which is why proactive maintenance is non-negotiable for any healthcare facility.
Beyond simple diagnostics, managing a fleet of flexible endoscopes requires a strategic understanding of their operational lifecycle and technical vulnerabilities. Whether you are addressing persistent issues like image clouding or evaluating the ROI of professional refurbishing, clarity is essential. In the following sections, we will provide a comprehensive technical breakdown: from the complex internal anatomy and specialized classifications of flexible scopes to a rigorous comparative analysis with rigid systems. Furthermore, we will examine the critical role of preventative maintenance protocols and establish a professional framework for selecting a repair partner that meets OEM-quality standards.
In modern clinical practice, a flexible endoscope is not a generic tool; it is a highly specialized instrument engineered to match the unique physiological challenges of different anatomical pathways. As a professional endoscopy equipment manufacturer, SIHANMED understands that the performance of these scopes relies on the intricate balance of their internal components—from the durability of the insertion tube to the precision of the bending section. Specialized providers such as arthroscopy instruments suppliers and flexible ureteroscope manufacturers also support healthcare facilities with tailored solutions.
GI endoscopy accounts for over 20 million procedures annually. These instruments are designed for the high-volume environment of the digestive tract, requiring robust materials and high-capacity channels.
Gastroscopes (Upper GI): Optimized for the esophagus and stomach. These scopes utilize high-density fiber optic bundles or advanced CMOS sensors to provide a panoramic view, essential for detecting ulcers and early-stage gastric cancers.
Colonoscopes (Lower GI): Significantly longer than gastroscopes, colonoscopes feature "Variable Stiffness" technology. This allows the physician to adjust the rigidity of the insertion tube to navigate the complex curves of the large intestine, minimizing patient discomfort.
Duodenoscopes: These are among the most complex flexible scopes due to their side-viewing optics and elevator mechanism. According to the FDA, the complexity of the elevator area makes these scopes "high-risk" for bioburden accumulation, requiring meticulous manual cleaning and high-quality distal end components to ensure patient safety.
_Endoscopes.jpg)
Respiratory scopes prioritize a slim profile and extreme maneuverability to access the distal branches of the lungs.
Bronchoscopes: Essential for diagnosing pulmonary infections and tumors. Their design focuses on micro-imaging chips and ultra-fine control wires that allow for precise tip deflection in narrow airways.
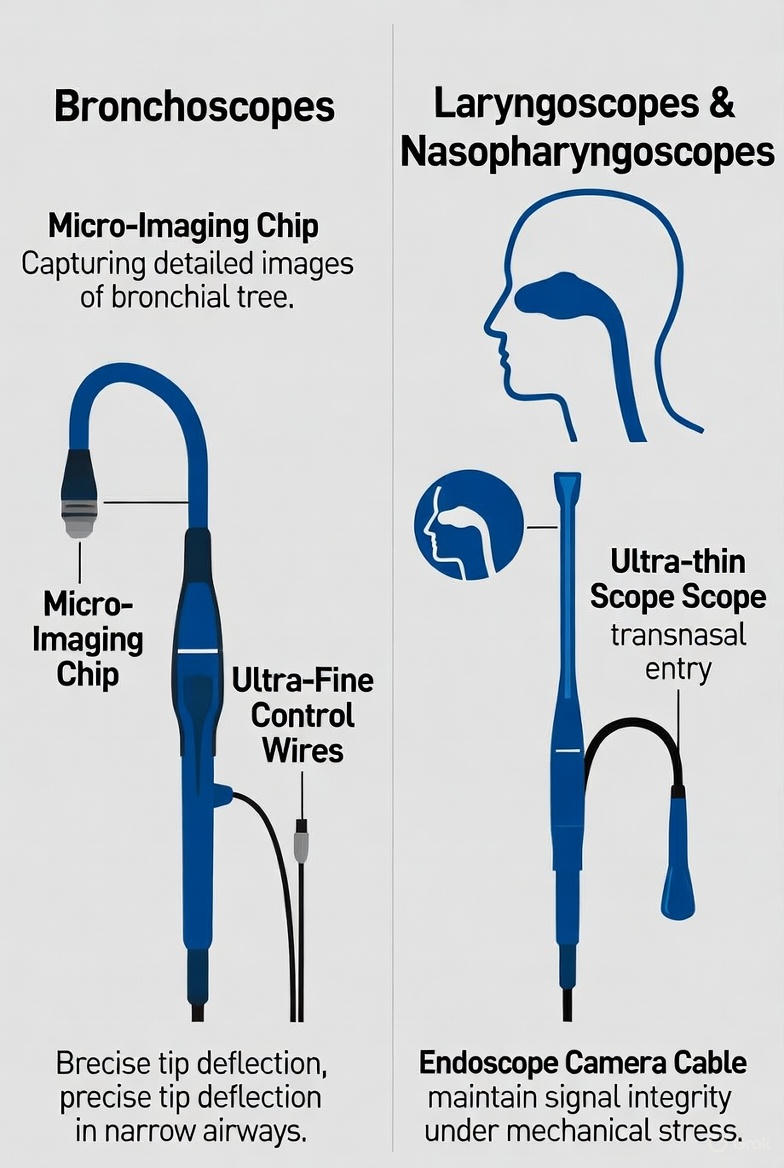
Laryngoscopes & Nasopharyngoscopes: These ultra-thin scopes are designed for transnasal entry. Their manufacturing requires specialized endoscope camera cables that can maintain signal integrity despite the constant mechanical stress of diagnostic navigation.
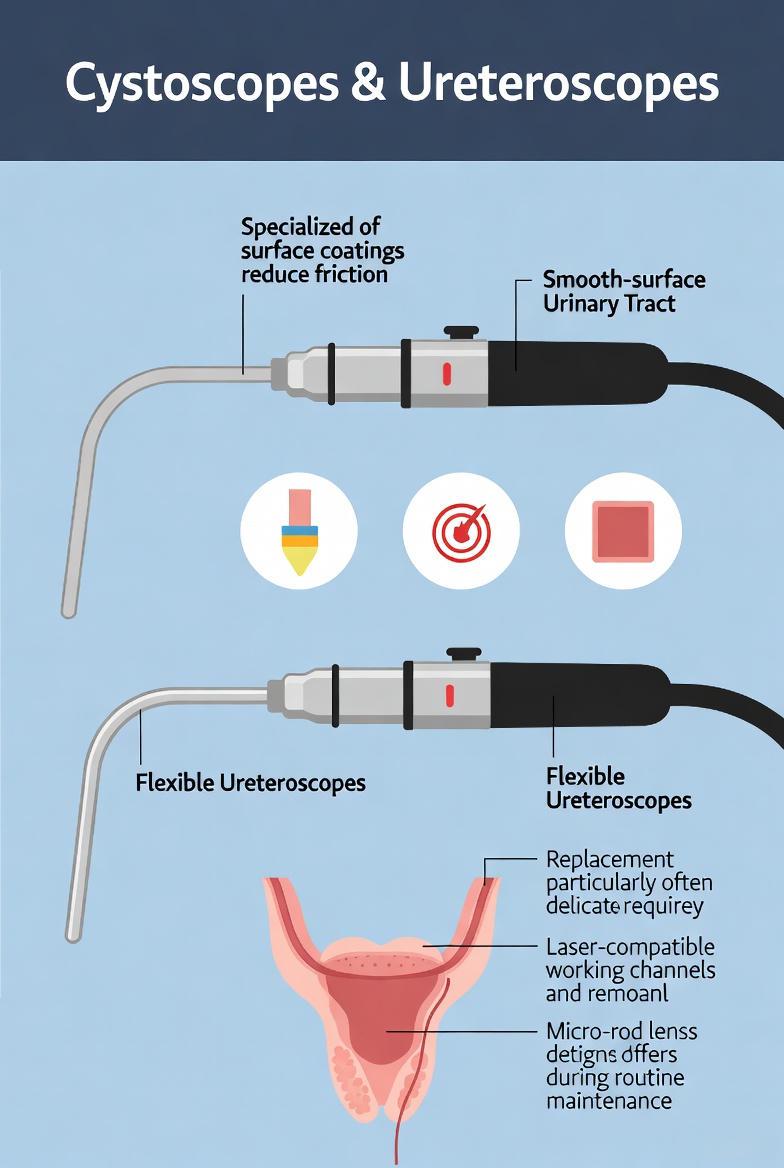
Cystoscopes & Ureteroscopes: Used within the urinary tract, these scopes require specialized smooth-surface coatings to reduce friction. Clinics often compare offerings from rigid cystoscope repair experts when evaluating options. Flexible ureteroscopes are particularly delicate, often requiring the replacement of laser-compatible working channels and micro-rod lenses during routine maintenance.
To maintain the integrity of these complex instruments, healthcare facilities must adhere to rigorous reprocessing standards. The ANSI/AAMI ST91:2021 guidelines emphasize that the longevity of a flexible endoscope is directly linked to the quality of its replacement parts and the precision of its leak-testing protocols. This includes using professional leak tools such as karl storz leak tester and zutron leak tester before each use.

To understand why a flexible endoscope requires precision-manufactured parts, one must look "under the hood." A single scope contains thousands of mechanical and optical components packed into a tiny diameter.
Here are some elements that define the internal makeup:
Insertion Tube
Light Guide Bundle
Distal Optics
The endoscope bending rubber is a key part of the flexible design, providing resilience to repeated articulation. Understanding flexible endoscope parts and function helps clinical staff recognize signs of wear before they escalate into costly failures.
Below is an enriched technical breakdown of the core components, their engineering functions, and the specific failure points that SIHANMED helps healthcare providers address through high-quality endoscope replacement parts.
| Component | Engineering Function | Critical Failure Points |
| Insertion Tube | Multi-layered polymer conduit designed for torque transmission and chemical resistance during HLD (High-Level Disinfection). | Fluid Invasion: Punctures or chemical degradation of the outer sheath leading to internal corrosion. |
| Bending Section | A vertebral mesh of interlocking rings controlled by high-tensile angulation wires for 4-way navigation. | Wire Fatigue: Stretching or snapping of Bowden cables, leading to "play" or loss of tip control. |
| Light Guide Bundle | Thousands of coherent glass fibers transmitting high-intensity cold light with minimal thermal dissipation. | Fiber Breakage: Cumulative mechanical stress causing "black dots" and progressive image dimming. |
| Biopsy/Suction Channel | Internal PTFE (Teflon) lining for instrument passage and fluid aspiration during procedures. | Occlusion & Kinking: Internal scoring or bioburden buildup that can harbor pathogens despite reprocessing. |
| Distal Tip | The optical terminal housing the CMOS/CCD sensor, objective lens, and air/water nozzles. | Seal Integrity Loss: The #1 cause of total scope failure due to fluid ingress into the video chip. |
The insertion tube is the most vulnerable part of the scope. Leading flexible endoscope manufacturers and professional endoscopy equipment suppliers like SIHANMED focus heavily on the "bend radius" and "torque stability." If the tube is too soft, it loops in the colon; if too stiff, it risks patient injury. Our replacement insertion tubes are engineered to maintain the original OEM elasticity while offering superior resistance to peracetic acid and glutaraldehyde—the leading causes of sheath thinning.
The bending section’s agility depends on the articulation mesh. Over time, repeated autoclaving or high-level disinfection can cause the metal "vertebrae" to wear down.
Specialist Insight: When the angulation wires stretch, the scope's "dancing" becomes uncoordinated. Replacing these with high-tensile stainless steel wires is essential to restore the 300°+ total range of motion required for complex retroflexion.
The distal tip is a micro-machined housing where the air/water nozzle and objective lens meet. According to FDA safety communications, the distal end—especially the elevator mechanism in duodenoscopes—is the most difficult area to clean. SIHANMED provides precision-engineered distal end components that ensure a watertight seal, preventing expensive CCD/CMOS sensor damage during the cleaning cycle.
Picture a fencing rapier (rigid) versus a whip (flexible). Both stabby, but only one bends. Here’s how they stack up:
Versatility: Like a yoga instructor, they twist where rigid endoscope can’t.
Patient Comfort: No need to "adjust" the body—just glide in naturally.
Multi-Purpose: Whether it’s lungs, intestines, or bladders, they do it all.
✔ Better Image Quality: No bending = no distortion.
✔ Durability: Fewer moving parts mean less breaking (unless you drop them).
Instruments like the Storz rigid endoscope are excellent in straight interventions where minimal angulation is required. When selecting hardware, clinics may explore options from a rigid endoscope supplier or rigid endoscope manufacturer that offer scopes tailored to specific specialties such as ENT or orthopedic use.
Final Verdict: Need precision in straight shots (like knee surgery)? Go rigid. Navigating the winding roads of the digestive tract? Flexibility reigns.
An endoscope’s lifecycle is not a linear path but a circular asset management cycle. During this cycle, choosing quality endoscope parts supplier relationships ensures access to both OEM and compatible components when replacement is necessary. Understanding the journey from "First Use" to "Professional Refurbishment" is critical for maximizing Return on Investment (ROI) while ensuring uncompromising patient safety. As a professional endoscopy equipment manufacturer, SIHANMED categorizes this lifecycle into four distinct phases focused on the Total Cost of Ownership (TCO).
When a brand-new endoscope enters clinical service, its optical clarity and mechanical feedback are at their zenith.
Performance Baseline: It is vital to record initial leak testing values and image resolution benchmarks during this phase.
Preventive Maintenance: Establishing a rigorous care protocol early on preserves the integrity of the OEM components for a longer duration.
Statistically, 90% of endoscope damage occurs outside the procedure room, specifically during the cleaning and disinfection cycle. Continuous exposure to High-Level Disinfectants (HLD) or liquid chemical sterilants eventually leads to material fatigue.
Chemical Degradation: Frequent immersion can cause the insertion tube sheath to thin, lose its coating, or develop micro-fissures.
Bioburden Risk: According to SGNA and AAMI ST91 standards, even microscopic scratches inside the biopsy channel can harbor bioburden, significantly increasing cross-contamination risks.
After 500 to 1,000 cycles, equipment typically enters a "sub-optimal" state where performance begins to degrade.
Common Symptoms: Restricted angulation (stretched wires), "black dots" in the image (broken fiber optics), or persistent leak test failures.
Manufacturer’s Insight: This is the most critical window for intervention. Timely replacement of the bending rubber or minor mechanical adjustments can prevent catastrophic fluid ingress, which would otherwise destroy the expensive CMOS/CCD sensor.
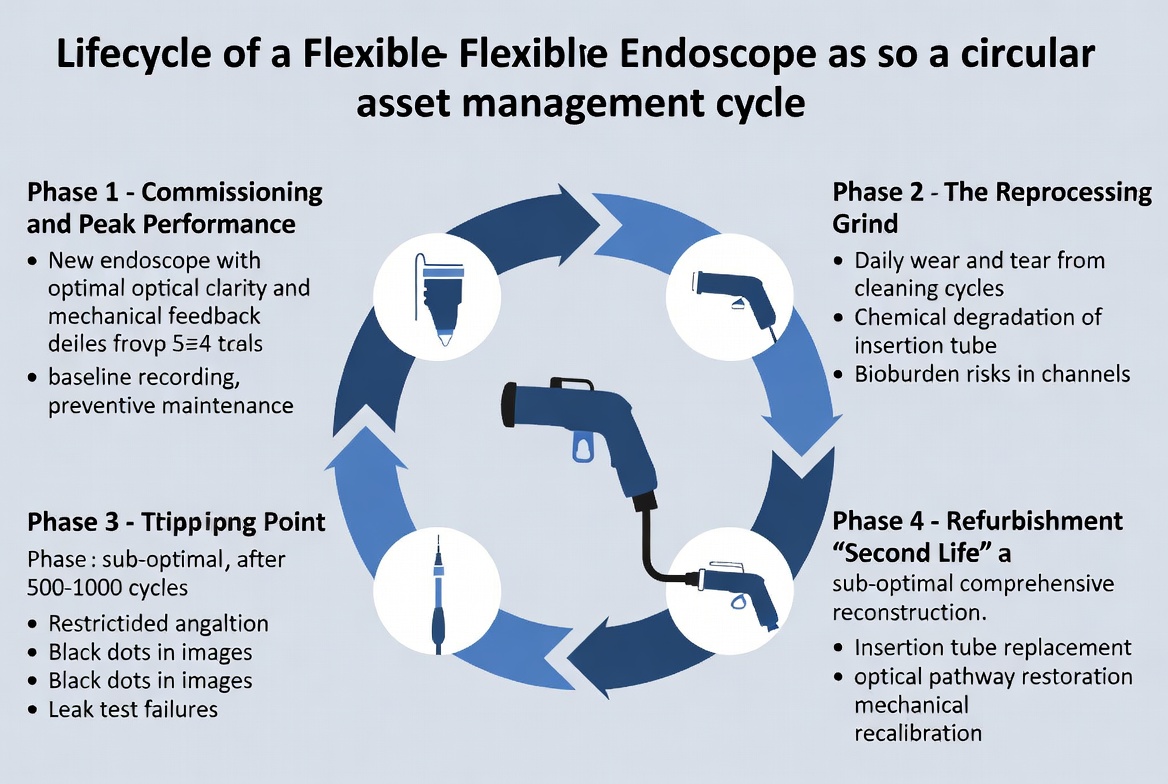
When a scope shows significant wear but the core imaging chip remains functional, professional refurbishment is a more sustainable and economical choice than purchasing new equipment.
SIHANMED Refurbishment Standards: Unlike basic repairs, our refurbishment process involves a comprehensive reconstruction:
Insertion Tube Replacement: Utilizing medical-grade polymers that meet or exceed OEM specifications for torque and flexibility.
Optical Pathway Restoration: Cleaning or replacing aged light guide bundles to restore over 95% of original light transmission.
Mechanical Recalibration: Re-tensioning angulation wires to restore the full rated degree of tip deflection.
Lifecycle Asset Comparison: New vs. Professionally Refurbished
| Metric | Brand New Equipment | SIHANMED Refurbished | Strategic Impact |
| Initial Cost (CapEx) | 100% | 40% - 60% | Significantly reduces capital pressure on medical facilities. |
| Optical Performance | Peak (Ultra-HD/4K) | Restored to OEM Standards | Dependent on high-quality sensors and light bundles. |
| Durability | High (Original Materials) | High (Enhanced OEM Parts) | SIHANMED parts offer superior chemical resistance to HLD. |
| ROI Cycle | Longer | Rapid | Ideal for high-turnover outpatient surgery centers. |
In the high-pressure environment of a surgical center, it is easy to overlook minor performance shifts. However, for a flexible endoscope, a minor "glitch" is often the precursor to a catastrophic failure that could cost thousands in repairs or, worse, compromise patient safety. When specific issues affect visual systems, technicians often review parts like endoscopy machine parts or specific camera assemblies before proceeding. Clinicians managing legacy Olympus systems may find themselves sourcing parts such as olympus wa33036a, olympus a22001a, olympus a22003a, or even olympus wa53005a when refurbishing scopes.
As a specialist endoscopy equipment manufacturer, SIHANMED recommends monitoring these five critical warning signs to determine when your device requires professional intervention.
The leak test is your first and most vital line of defense. A failed test indicates a breach in the scope’s watertight integrity.
The Danger: Even a "slow leak" allows enzymatic cleaners and moisture to enter the internal cavity, leading to the rapid corrosion of the angulation wires and the delicate CMOS/CCD image sensor.
Proactive Action: If a scope fails a leak test, it must be pulled from service immediately—before it undergoes high-level disinfection (HLD).
When you turn the control knobs, the distal tip should respond with crisp, immediate movement.
The Danger: If the knobs feel "spongy," have excessive "play," or cannot reach their full rated degree of deflection (e.g., 210° up/90° down), the internal angulation wires (Bowden cables) have likely stretched or the articulation mesh is worn.
Proactive Action: Professional re-tensioning or wire replacement can restore full maneuverability and prevent a mid-procedure mechanical lock-up.
Your image quality is a direct reflection of the scope’s internal health.
Cloudy/Blurry Image: This often indicates "fogging" inside the objective lens, a clear sign of a failed seal and fluid invasion.
Black Dots: In fiber-optic scopes, black dots represent broken glass fibers in the image bundle. In video scopes, flickering or color distortion points to a failing endoscope camera cable or a damaged sensor chip.
Proactive Action: Early cleaning of the optical pathway or cable replacement is far more cost-effective than replacing a short-circuited CCD sensor.
The insertion tube must be smooth and free of any physical defects.
The Danger: Look for "bubbling" on the surface, "scaling" from chemical exposure, or deep kinks. According to AAMI ST91:2021 standards, these physical defects can harbor bioburden and multi-drug resistant organisms (MDROs) that are impossible to remove through standard reprocessing.
Proactive Action: Replacing a worn insertion tube sheath restores the scope's biocontainment integrity and ensures smooth, friction-free entry.
If a biopsy forcep or snare feels "tight" or gets stuck while passing through the scope, the internal channel is compromised.
The Danger: This usually indicates a kinked or scored biopsy channel. Internal scratches can trap organic debris, leading to cross-contamination risks flagged by the FDA.
Proactive Action: A channel replacement is a routine maintenance task that prevents internal tearing and potential "scope-flooding" accidents.
In addition, industry repair training resources such as endoscope repair training or rigid endoscope repair training help technicians expand their capabilities.
Maintenance Checklist: When to Call SIHANMED
| Symptom | Urgency | Recommended Service |
| Moisture inside the lens | CRITICAL | Immediate seal repair & CCD drying. |
| Loose control knobs | HIGH | Angulation wire re-tensioning/replacement. |
| Surface scratches on tube | MODERATE | Insertion tube polishing or re-sheathing. |
| Dim light output | MODERATE | Light guide bundle replacement. |
In a clinical setting, neglecting endoscope maintenance is not merely a service oversight; it is a significant risk to patient safety and a drain on hospital finances. While casual comparisons to luxury car maintenance are common, the reality of endoscopic asset management involves complex bio-mechanical and regulatory factors.
As a dedicated endoscopy equipment manufacturer, SIHANMED emphasizes that proactive maintenance is the primary driver of high diagnostic accuracy and infection control.
A flexible endoscope is only as valuable as the image it produces. Over time, friction and improper handling cause microscopic scratches on the distal lens and breakage of internal light guide fibers.
The Impact: These defects cause light scattering and "noise," which can lead to the misinterpretation of subtle mucosal changes, such as early-stage gastric cancers or small polyps.
Expert Insight: Professional recalibration of the optical train ensures that HD and 4K sensors maintain their native resolution throughout the device's service life.
The "Seal Integrity" of a scope is its most vulnerable feature. A breach as small as a few microns is enough for high-level disinfectants (HLD) to penetrate the internal cavity.
The Financial Risk: Once fluid enters, it causes rapid corrosion of the angulation wires and fatal short-circuiting of the CCD/CMOS sensor. What could have been a $500 seal replacement often escalates into a $10,000+ total overhaul.
Clinical Safety: Fluid ingress can also harbor chemical residues that are potentially toxic to the next patient.
The internal biopsy and suction channels are prime environments for microbial proliferation. If these channels are scored or scratched, they become impossible to fully disinfect.
The "Biofilm" Factor: According to ANSI/AAMI ST91:2021, bacteria can form resilient biofilms within damaged channels, protecting them from chemical sterilants.
Infection Control: Adhering to strict maintenance protocols is essential to prevent the transmission of multi-drug resistant organisms (MDROs), a top priority for FDA and SGNA compliance.
Proper cleaning and prompt, minor repairs can significantly extend a scope’s operational lifespan, often doubling it from 5 to 10 years.
Budget Strategy: By shifting from a "reactive" repair model to a "proactive" maintenance model, healthcare facilities can stabilize their Capital Expenditure (CapEx) and avoid the disruption of unexpected equipment downtime.
Asset Longevity: Professional refurbishment using OEM-quality replacement parts ensures that the device operates within its original safety parameters, delaying the need for expensive fleet replacements.
Summary: The Value of Precision Care
| Risk Category | Neglect Outcome | Maintenance Benefit |
| Diagnostic | Blurred/Dim Images | High-Fidelity Visualization |
| Mechanical | Fluid Invasion & Corrosion | Extended Component Life |
| Safety | Cross-Contamination Risk | Full Regulatory Compliance |
| Financial | High CapEx / Early Replacement | Optimized TCO & ROI |
Selecting an appropriate repair partner is crucial. Reputable partners not only provide quality service but often list endoscopy scope parts and endoscope parts for sale on demand, ensuring ready access to necessary components. Picking an endoscope repair services company shouldn’t feel like swiping on Tinder. Here’s how to avoid heartbreak:
"Do you use OEM-compatible parts?"
Knockoff parts are like dollar-store duct tape—cheap, but the fix won’t last.
"Can you provide before/after repair reports?"
No receipts? No trust.
"Do you offer loaner scopes during repairs?"
Because downtime shouldn’t mean no-time.
"Are your technicians factory-trained?"
Would you let a YouTube-certified mechanic fix your Porsche?
"What’s your average turnaround time?"
A "few weeks" could mean your OR gathers dust.
Pro Tip: If their answer to any question is “Trust us,” run. Fast.
Rigid endoscope vs flexible endoscope comparisons highlight that rigid ones are suited for straight-line procedures like arthroscopy due to their durability and image clarity, while flexible endoscopes excel in navigating curved paths for flexible endoscope uses such as gastrointestinal exams.
Flexible endoscope uses span diagnostics in the digestive and respiratory systems, biopsies, and therapeutic interventions, making them essential for non-invasive procedures where flexibility is key.
Flexible endoscopy is a minimally invasive technique using a flexible endoscope to visualize and treat internal issues, often what is flexible endoscopy refers to procedures like colonoscopies that prioritize patient comfort and accuracy.
What is a flexible endoscope encompasses a device with a pliable tube, camera, and light for internal viewing, distinguishing it from rigid models in its ability to bend and adapt.
In flexible vs rigid endoscopy decisions, flexible options are preferred for winding anatomy like the intestines, offering versatility, whereas rigid endoscopy provides precision in linear areas.
Flexible endoscope parts and function include the insertion tube for entry, optics for imaging, and controls for navigation, all integrated to ensure effective performance during exams.
The flexible endoscope structure features layered materials and articulating sections that allow bending without compromising image quality or durability.
An endoscope flexible is ideal for procedures requiring navigation through body curves, providing real-time visuals that rigid versions cannot match in complex anatomies.
The structure of flexible endoscope includes fiber optic bundles, control mechanisms, and protective sheathing, all engineered for safe and efficient internal exploration.
Flexible endoscopes are favored for their adaptability in specialties like gastroenterology and pulmonology, reducing invasiveness and improving diagnostic outcomes.
References & Clinical Guidelines
The technical standards and safety protocols discussed in this article are based on the latest guidelines from globally recognized medical and regulatory organizations.
[1] ANSI/AAMI ST91:2021 – Flexible and Semi-Rigid Endoscope Processing
[2] FDA Safety Communication: Reprocessing Medical Devices
[3] SGNA Standards of Infection Prevention.
[4] Multi-Society Guideline on Reprocessing Flexible GI Endoscopes (GIE Journal)
[5] AORN Guideline for Perioperative Practice
You May Like:
Sterilization of Endoscope Is Done by Which Solution

With years of dedication to the medical equipment industry, Shengjun He has leveraged his solid professional expertise and keen insight into industry trends to establish Sihan Medical as a leading force in the endoscope repair sector. Prior to founding Sihan Medical, he accumulated extensive experience in medical device maintenance—a foundation that proved instrumental for his entrepreneurial journey. His background spans hands-on equipment repair, technical R&D, and management, granting him comprehensive understanding of medical devices, from their underlying technology to market demands.
This is the first one.


